


Q&A
What is ionising radiation? How is radiation involved in medicine?
Radiation is the emission of energy from a source. If the energy is enough to eject electrons from an atom in matter, the radiation is called ionising radiation. Exposure to small doses of radiation is a natural and constant part of our environment. Human beings are exposed to cosmic radiation as well as naturally appearing radioactive materials found in soil, water, air and food[1].
On the other hand, the use of radiation in medicine is the largest human-made source of radiation exposure today. Ionising-radiation sources for medical procedures are typically man-made. These can be tracers, which emit gamma rays, in radiopharmaceuticals administered to patients to allow for their distribution to be analysed by nuclear medicine equipment or X-rays artificially produced by tubes in various X-ray equipment.
How much radiation is used in X-ray exams?
The radiation dose varies according to the specific procedure, quality of the image needed for diagnosis, size of the patient, difficulty of the procedure, and settings of the imaging equipment. Common to all imaging facilities is the principle to keep doses as low as reasonably achievable.
Is medical radiation associated with a certain risk?
When a radiological imaging procedure is justified and optimised, the benefit to the patient should outweigh any risk. For this reason, there is no limitation to the relatively small radiation doses used to diagnose and manage disease. Radiation risks from the low radiation doses used in diagnostic radiology procedures are generally small.
What are the consequences of not doing the procedure?
Radiological imaging procedures are intended to contribute to a timely and accurate diagnosis to convalesce health outcomes. The consequences of not undergoing requested procedures may affect the health outcome in terms of an incorrect or delayed diagnosis.
Which medical imaging procedures do not use ionising radiation?
Two common imaging techniques that do not utilize ionising radiation are US and MRI.
What are the benefits versus the risks?
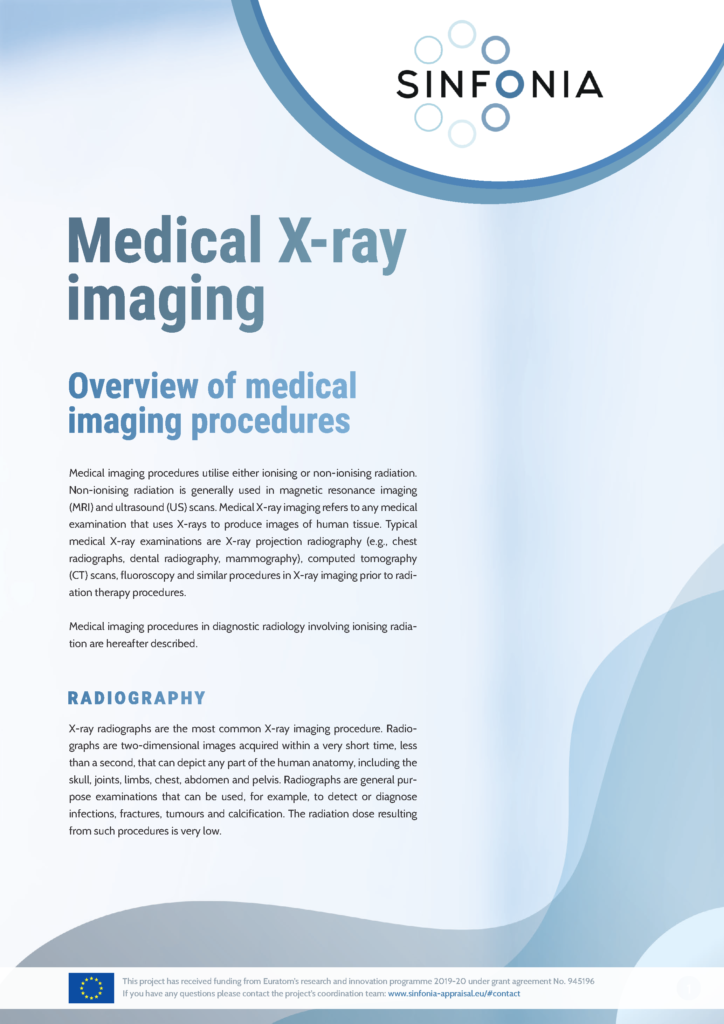
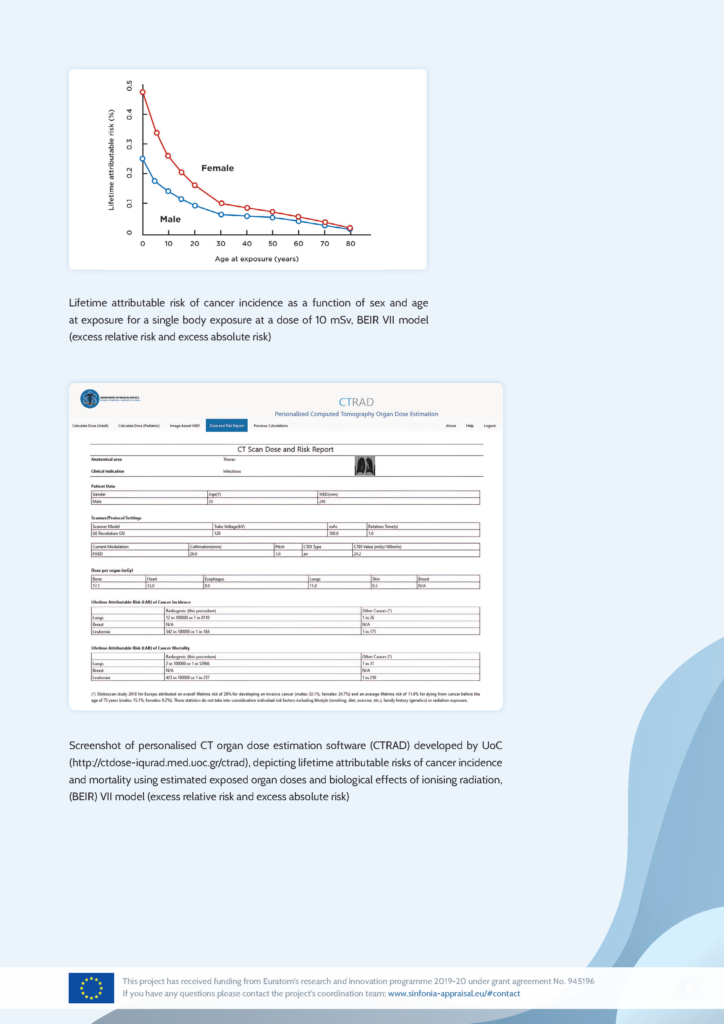
The benefits of medical imaging include accurate diagnosis, precise guidance of therapy, and monitoring of disease progression. Radiation risks from the low radiation doses used in diagnostic radiology procedures are generally small. The chance of developing cancer over the course of a lifetime is more than 1 in 3 in epidemiological studies alone. Nevertheless, an increased, albeit very low, risk of cancer development in people exposed to low radiation doses associated with diagnostic radiology procedures has been reported.
How will I know if the right radiation dose is used for my imaging procedure?
Many techniques may often lower the dose and risk in X-ray medical imaging without compromising the diagnostic quality of the images. The actual dose varies according to the patient’s size and additional required information. Useful guidance for imaging facilities is available through national and international sources, and, in most countries, reference values called diagnostic reference levels (DRLs) are outlined for typical examinations as tools for optimisation and quality assurance.
I find different quantities and units for ionising radiation doses in various sources. What are these units, and how are they connected with the associated risk?
A quantity of the ionising radiation used during a medical X-ray procedure can be absorbed by human tissue. The radiation dose is the amount of energy absorbed per unit mass in the exposed tissues and organs and is measured in units called the gray (Gy). During most X-ray imaging procedures, the absorbed dose is very low, usually measured in milligray (mGy), which is three orders of magnitude lower than the Gy. For comparison, the dose delivered during radiation therapy is on the order of several tens of Gy.
Risks due to exposure to different radiation types can be compared in terms of equivalent dose. The effective dose is the weighted sum of the equivalent doses in a number of tissues, using tissue-specific weighting factors, which reflect an approximation of their relative sensitivity to radiation-induced cancer. The effective dose was not intended to give an accurate estimate of the risk of radiation effects for individuals undergoing medical radiation procedures. For individual risk assessment as well as epidemiological studies, the organ dose, either absorbed or equivalent organ dose, would be a more appropriate quantity. The unit of equivalent and effective dose is the sievert (Sv). In diagnostic X-ray imaging it is more practical to express doses in terms of mSv.
[1] The average annual radiation exposure from all sources for the world population is approximately 3 mSv/year per person.
Glossary
Angiograph – a special kind of medical test that uses X-rays and a contrast agent to take pictures of blood vessels in the body, helping doctors see if there are any blockages or problems.
BEIR VII model – a scientific framework developed by the National Research Council’s Committee on the Biological Effects of Ionizing Radiation (BEIR). It provides guidelines and estimates for the health risks associated with exposure to ionizing radiation, helping inform radiation protection standards and policies.
Cardiac catheterization – a medical procedure where a thin tube (catheter) is inserted into the heart’s blood vessels to diagnose or treat heart conditions, often using contrast agents and X-rays.
Contrast agent – a substance used in medical tests to make certain parts of the body easier to see in pictures, helping doctors detect and diagnose problems.
Epidemiological studies – research investigations that focus on understanding the patterns, causes, and effects of health and disease conditions in specific populations, helping identify factors that contribute to public health.
Interventional procedure – a medical technique where doctors use instruments like catheters or needles to diagnose or treat conditions inside the body, often guided by imaging methods like X-rays.
Invasive cancer – a type of cancer that has grown beyond its original location and has the potential to spread to nearby tissues or other parts of the body.
Magnetic resonance imaging – a medical imaging technique using magnetic fields to provide images of the anatomy of the body.
mSv – stands for millisievert, which is a unit of measurement for radiation absorbed by the human body.
Ultrasound – a medical imaging technique that uses high-frequency sound waves to create real-time images of the inside of the body, helping doctors visualize organs, tissues, and blood flow without using radiation.
X-ray cone beam computed tomography – a type of medical imaging that uses a cone-shaped X-ray beam to create three-dimensional images of structures.
Link to the Glossary of the International Commission for Radiation Protection (ICRP): ICRP Glossary – ICRPaedia